Self management strategies
Spasticity in Neurology conditions is usually a life long issue. It can fluctuate over time and worsen if not managed well. Learning effective self management strategy techniques can help to maintain and even improve spasticity. There are various ways of self managing that may prove beneficial.
Daily movement and Stretching
Regular movement is one of the most effective ways to manage spasticity. Keeping your joints and muscles moving helps reduce stiffness and prevents long-term tightening.
What you can do:
- Perform gentle daily stretches for affected muscles.
- Move each joint through its comfortable range — slow, steady movements work best.
- Try to include both sides of the body to support balance and posture.
- Use breathing techniques (slow, steady breaths) to help the muscles relax during stretching.
- Your physiotherapist can provide a personalised programme if needed.
Why it helps:Stretching reduces tightness, helps muscles relax more easily, and lowers the risk of developing contractures or joint pain.
Positioning
How you sit, lie or stand can influence spasticity levels. Good positioning can reduce discomfort and help prevent posture-related issues.
Tips for better positioning:
Sitting: Keep feet flat on the floor, hips level, back supported and avoid leaning to one side. For arm spasticity, consider pillow support to protect shoulder joint and allow muscles to relax.
Lying: Use pillows to support comfortable positions. Some people benefit from a pillow between the knees or under the calf. Pillows under an affected arm can also help.
Standing/walking: Use supportive footwear and consider pacing activities to avoid fatigue.
Change position regularly — ideally every 1–2 hours.
Why it helps:
Poor posture increases muscle tension, while supported, comfortable positions reduce unwanted tightening.
Managing triggers
Spasticity often worsens when the body is under stress or discomfort. Recognising and managing triggers can reduce flare-ups.
What you can do:- Stay hydrated and maintain regular bowel habits.
- Dress in soft, loose, comfortable clothing.
- Address pain early with appropriate strategies or advice.
- Plan for good sleep routines and rest breaks.
- Keep warm in cold weather.
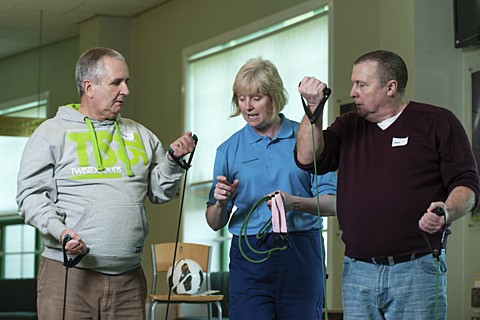
- Exercise and Physical Activity.
Staying active helps manage tone, reduces stiffness and supports overall wellbeing. Safe ways to stay active include gentle walking, cycling, or seated exercise and strengthening exercises for weaker muscles, including activities such as Pilates, yoga or tai chi. Exercise little and often to pace your fatigue levels and avoid becoming too tired.
Why it helps:Regular activity keeps muscles healthy, supports posture, improves circulation and reduces reflex over-activity.
Relaxation techniques
Simple strategies can help relax muscles and reduce stiffness or spasms.
Options include:
- Warmth: Warm towels, showers or baths (avoid high heat that irritates skin).
- Relaxation techniques: Slow breathing, guided relaxation or mindfulness.
- Gentle massage to relax surrounding muscles.
- Weight-bearing positions (e.g., standing with support) which can help calm the stretch reflex.
Why it helps:Relaxation reduces nervous system excitability and helps muscles let go.
Managing fatigue
Fatigue can increase spasticity and make everyday tasks harder.
Helpful strategies:
- Pace yourself and break tasks into smaller steps.
- Prioritise key activities and plan rest breaks.
- Try to keep a steady routine for activity, rest and sleep.
- Use energy-saving techniques such as sitting for tasks when possible.
Staying comfortable with splints and equipment
Some people use splints, orthotics or seating supports to help manage spasticity.
Self-management for equipment:
- Check straps for tightness.
- Ensure skin remains healthy — look for redness or pressure marks.
- Clean equipment regularly.
- Follow the wearing schedule recommended by your orthotist/therapist.
When to seek help
You should contact your physiotherapist, GP or specialist team if you notice:
- A sudden or significant increase in spasticity.
- New spasms or severe pain.
- Signs of infection.
- Changes in bladder or bowel function.
- Difficulty completing daily activities you were managing before.
- Reduced movement or new joint stiffness.
- Skin changes or pressure areas.
- Early support can prevent further complications.
Carers can help too!
Carers and family members can help with stretching, positioning, movement and spotting triggers. Providing them with clear guidance helps keep you safe and comfortable.
Carers may help by:
- Assisting with stretches safely if unable to manage independently.
- Supporting good positioning in bed/chair.
- Checking for triggers.
- Encouraging regular activity.
- Helping with routines such as hydration, comfort and rest breaks